Combination therapies and synergistic approaches refer to the use of multiple treatments or interventions together to enhance their effectiveness in addressing a disease. This approach is employed in various fields of medicine, including cancer, infectious diseases, and mental health.
Monoclonal antibody (mAb) therapeutics have been successfully developed and commercialized for various indications, including the neutralization of toxins, bacteria, and viruses. However, mAb potency is lower than traditional polyclonal antibodies (pAbs), and its efficacy may be significantly hindered by any absences or changes of its target epitope in a mutant or subtype of the infectious agent. These constraints can be overcome through the use of combination therapies, such as oligoclonal mAb combinations with different specificities to the target antigen.1
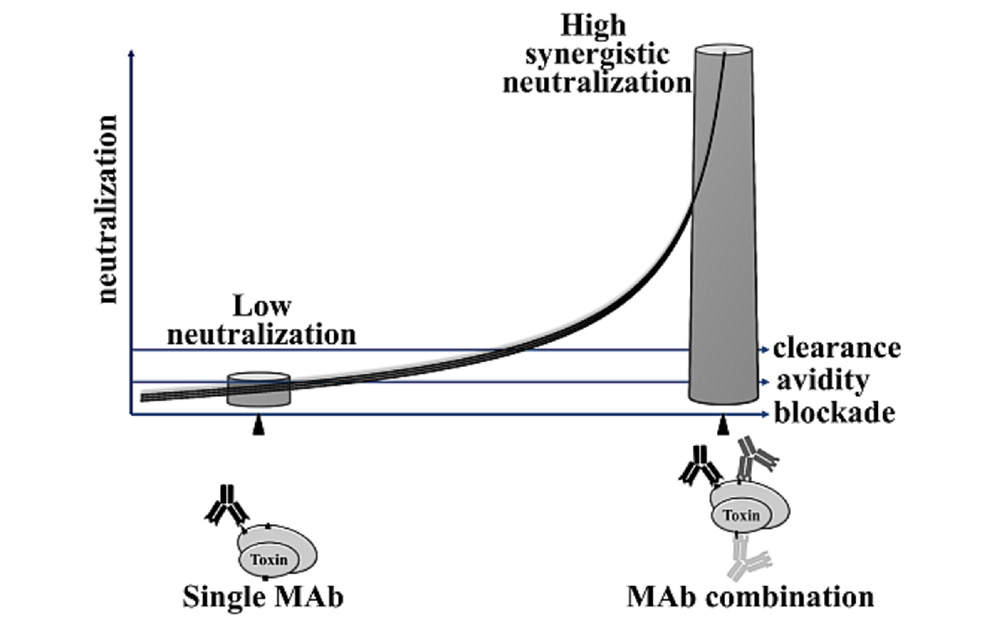
Combinations of mAbs against infectious agents show increased efficacy and synergistic enhancement, with some cases surpassing the efficacy of the pAb-based therapies. Diamant et al. (2015) describe three reasons for this:
- Simultaneous binding of mAbs to multiple functional sites of the toxin helps block at least two epitopes that react with the target cell, thus reducing toxin potency.
- There is an increase in affinity of the combination of mAbs compared to single mAb components.
- Fc-mediated clearance of antibody-toxin ICs from serum is enhanced by multimeric antibody Fc decoration of the toxin.
These advantages have been demonstrated through several studies from the past 30 years. An example of an oligoclonal antibody-based preparation was the production of mAbs against botulinum neurotoxins (BoNT). Researchers found significant synergistic neutralization by the combined anti-BoNT mAbs, which is an optimistic finding as current treatments for botulism depends on equine or human pAb-based antitoxin therapy.2
Antibody combination therapies are not limited to mAbs, however, with advancements in antibody engineering allowing for different formats. For example, researchers recently developed an anti-TGF-β/VEGF bispecific antibody, which showed synergistic efficacy in combination with PD-1 blockade. This Y332D antibody was developed because blocking the PD-1/PD-L1 axis alone was not enough to restore normal immune response. Instead, Y332D was more effective in inhibiting tumor growth and metastasis over anti-TGF-β and anti-VEGF monotherapies.3,4
- Diamant, E., Torgeman, A., Ozeri, E., & Zichel, R. (2015). Monoclonal Antibody Combinations that Present Synergistic Neutralizing Activity: A Platform for Next-Generation Anti-Toxin Drugs. Toxins, 7(6), 1854-1881. https://doi.org/10.3390/toxins7061854
- Dembek, Z. F., Smith, L. A., & Rusnak, J. M. (2007). Botulism: cause, effects, diagnosis, clinical and laboratory identification, and treatment modalities. Disaster medicine and public health preparedness, 1(2), 122–134. https://doi.org/10.1097/DMP.0b013e318158c5fd
- Niu, M., Yi, M., Wu, Y. et al. Synergistic efficacy of simultaneous anti-TGF-β/VEGF bispecific antibody and PD-1 blockade in cancer therapy. J Hematol Oncol 16, 94 (2023). https://doi.org/10.1186/s13045-023-01487-5
- Sun, JY., Zhang, D., Wu, S. et al. Resistance to PD-1/PD-L1 blockade cancer immunotherapy: mechanisms, predictive factors, and future perspectives. Biomark Res 8, 35 (2020). https://doi.org/10.1186/s40364-020-00212-5